My story began at just 8 years old
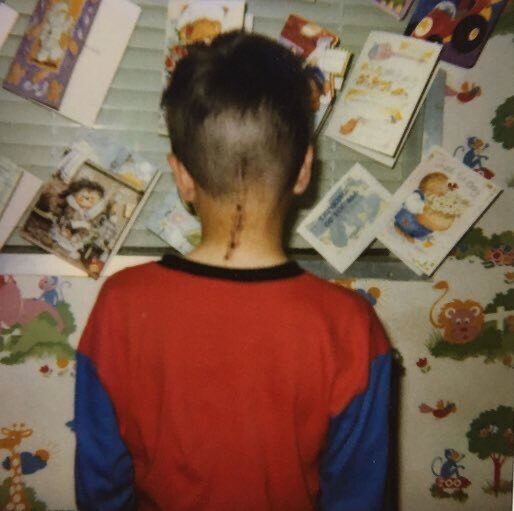
When I was 8 years old in 1998, I had a brain tumour removed from the back of my head. The tumour was benign, but two years later I needed a VP shunt fitted due to the build up of pressure in my head (A VP shunt is a mechanical device that relieves pressure in the head by draining excess cerebrospinal fluid into a cavity in the abdomin).The pressure was caused by an obstruction in the flow of cerebrospinal fluid (CSF)
I had a few complications with the shunt in the first few years of having it fitted, but for the next 10 years or so I was relatively well, although I did have a bout of meningitis in 2009. Whilst in hospital for the meningitis I underwent ICP monitoring (where a device called an ICP Bolt is used to measure pressure within the head) which confirmed the pressure in my head was stable. I developed slight hearing loss around 2012 which was always attributed to the episode of meningitis in 2009, but other than that I was relatively well.
A rude awakening
In mid-August 2015, I woke up in the middle of the night with a high-pitched screeching sound in my right ear, the worst headache I’d had for many years, and my right ear was popping, like I had just taken off in an aeroplane.
I took some painkillers and eventually the screeching sound and headache subsided, so I went back to sleep. When I woke up in the morning to go to work, my right ear was still popping, and I couldn’t do anything to resolve it. Yawning, gulping water and sucking a boiled sweet didn’t help at all. I went to my local audiologist who said I had a 20db hearing reduction in my ear, so he referred me to the ENT department at the hospital, but a few days later I began to get very dizzy on my feet and struggled to stay upright for prolonged periods of time.
VP shunt problems
I hadn’t had an issue with the shunt since 2002. It was now 2015, and I suddenly found myself having to have an operation to unblock it to relieve the pressure. My gut feeling was telling me there was more to this than just the shunt, after all I’d been well for many years, so why would it suddenly block?
After I had the operation to unblock the shunt, I was discharged from hospital, my ear was still popping, and I had more frequent headaches and dizziness. Multiple trips to A&E and numerous CT scans gave me no answers and this was probably one of the most stressful experiences that I have ever been through. That feeling when you know something is wrong, but the doctors have no idea where to look is a scary situation to be in. Part of the problem I think, was that I had a shunt, and it was the ‘go-to’ area whenever I developed any neurological symptoms.
A diagnosis - is this it?
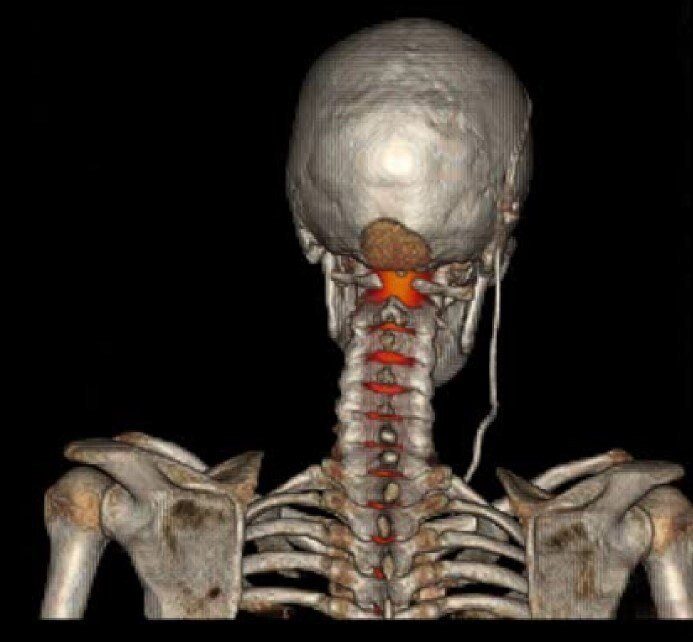
2016 was a manic year for me. I saw 4 different neurologists, ENT specialists, a few neurosurgeons and eventually got a diagnosis of an ultra-rare neurological condition called superficial siderosis (SS).
I’d missed so much work and was really struggling to stay upright for any length of time. I’d been searching the internet and talking to people all around the world to find out if superficial siderosis was causing my symptoms. I could no longer play music in my band due to my ongoing issues. I often asked other superficial siderosis patients if they had popping in their ears or found relief from the symptoms when lying flat; and the answer was always no. This prompted me to keep searching to see if there were other things going on.
Tests, tests and more tests

In 2017 I underwent ICP monitoring which showed the pressure in my head was significantly low.
ICP (intracranial pressure) monitoring is when a 'bolt' with electrodes attached is inserted into your brain to measure the pressure inside over a period of time.
Again, the go to area was my shunt, but at least it was now confirmed that I had low pressure in my head (intracranial hypotension). My surgeon decided to change the valve on my shunt to a newer model with a built-in anti siphon device. The theory was that my shunt was draining too much CSF and was causing low pressure. This new shunt valve was adjustable, and the resistance could be changed non-invasively by using a magnet. Week after week, I was back and forth to the hospital having the shunt valve adjusted so that the shunt would drain less CSF. The only problem was that it was having little to no effect on my symptoms.
A change of plan
At the latter end of 2017 my surgeon decided to move away from the shunt and focus on the back of my head where I had the tumour removed as a child. By now I’d developed the popping sensation in my left ear as well as the right, and I also had some further hearing loss. However, it’s probable that the hearing loss was also due to the superficial siderosis, although the same cannot be said of the popping in my ears.
An MRI scan showed I had a large pseudomeningocele at the site where I had the tumour removed when I was 8 years old (A pseudomeningocele is an abnormal collection of CSF outside of the dura which is the membrane that covers the brain and spine).
Although the MRI scan did not show that the pseudomeningocele was leaking, my surgeon decided he would operate to repair it, in the hope that it would resolve the low pressure in my head. On 5th of December 2017, I went in for neurosurgery to have the pseudomeningocele repaired and had an ICP monitor fitted to see if the pressure in my head increased following the surgery. The pressure readings on the ICP monitor did not increase and my symptoms did not get any better, so my surgeon said to give it some time to see if it resolved.
Back to the drawing board
It was now a month since the attempted pseudomeningocele repair, and my symptoms were as relentless as ever. I was unable to attend work due to the need to lie flat most of the day, and I was mentally struggling with not being able to do anything. My surgeon decided he would arrange for me to have a CT myelogram to see if the back of my head was leaking. I was pleased to see a new approach was being taken, as I had read this was one of the best ways to find and locate a leak, if there was one. I had the CT myelogram, but it did not show a leak. I was quite stumped at this point, so I decided to look at what other options I had.
CT Myelogram - This is a procedure where contrast dye is inserted into the CSF via a lumbar puncture and followed by a CT scan. The dye can help to highlight any defects when the scan is carried out.
A second neurosurgical opinion
By now I was nearly completely deaf, in constant pain and really struggling to get by, so I decided to seek a second opinion from a neurosurgeon in a different health board area. It was early February 2018 and I paid privately for a consultation, as I really felt like I was going around in circles. The surgeon I saw privately had all my medical records from my regular surgeon. He was satisfied with the care I had been given and could only recommend adding an anti-siphon device to my shunt. I was quite disappointed with this as I was adamant it wasn’t the shunt causing the low pressure and saw it as a big set back because another surgeon was suggesting investigating the shunt again.
Back to the shunt again
Back at the regular hospital, my surgeon decided he would ‘tie off’ the shunt to see if it stopped the low pressure. This involved making a kink in the shunt tubing so it would no longer drain excess CSF, and hopefully compensate for the CSF that I was losing due to the shunt ‘over-draining’. Once again, I had an ICP monitor fitted to record the change in pressure whilst the shunt was tied off.
I went in for the procedure, which was very minor surgery. My surgeon made a kink in the shunt tubing in my chest area whilst his registrar fitted the ICP bolt at the same time. I can’t remember anything after this as I had developed what I was told was ‘low pressure hydrocephalus’. A day or so later, the shunt was untied, and it was time for the next instalment of this ever-prolonged saga.
The gravitational anti-siphon device
My surgeon decided to listen to what his colleague at the other health board had suggested and went on to fit a standalone gravitational anti-siphon device on the shunt tubing in my chest area. This was a simple operation that took around 15 minutes and came with no complications like when I had the shunt tied off. The only issue now was I found myself back and forth having the anti-siphon device adjusted week after week, and just like the shunt valve in my head, it had no effect on the low-pressure symptoms. This prompted me to use the CSF leak help group on Facebook to plan my next move.
It always gets worse before it gets better
I’d contacted one of the renown CSF leak experts mentioned in the CSF Leak Facebook group and managed to get an appointment in September, but in mid-August the back of my head began violently throbbing. My parents took me to my local hospital A&E where the doctor was adamant it was the result of extreme low pressure in my head. A CT scan was carried out that showed my ventricles were so small that they were close to collapsing. A neurologist came to see me and tilted my bed backwards so that my head was lower than my feet. I was given IV fluids and the neurologist pushed for me to be admitted to the neurosurgery ward at my usual hospital. Whilst I was lying in bed in the local hospital, a superficial siderosis (SS) expert in the U.S.A emailed me to suggest my surgeon look to open the back of my head and repair the pseudomeningocele, as he believed it could be the source of the low pressure, and the bleed that caused the SS.
I was eventually blue lighted to the neurosurgery ward at the other hospital in the middle of the night.
A CT cisternogram
My regular surgeon was on annual leave, and upon returning a few days into my admission, he attempted to adjust the anti-siphon device in my chest, but it was stuck. Another surgeon came to see me early the following morning and said he had spoken to my surgeon and asked him to move away from the shunt, and that they were going to go back to looking for a leak. Moments later my surgeon came in and advised of a CT cisternogram. A procedure which is the same as a myelogram, where contrast dye is inserted into the spinal fluid via a lumbar puncture, the only difference is that the head is scanned as well as the spine.
The procedure was carried out, and shortly afterwards my surgeon came into my room to say that it had located a leak. He pointed at the back of his head and said, ‘you have a leak’, and went on to say there was a 6cm hole at the back of my head where the tumour had been removed. One of the nurses then came into my room and gave me a high five and said, “you had been saying it was a leak for over a year!.”My surgeon then came back to explain he would order a custom-made implant using the dimensions from my MRI scans to fill the cavity at the back of my head. I was discharged and on call to be readmitted for surgical repair.
In the meantime
Whilst on call to have the back of my head sealed with the implant, my dad and I took a trip to see the renowned CSF leak expert in the Midlands. I must say, I was very impressed with both the questions he asked and the examinations he performed. At the time I had a soft patch of swelling at the side of my head as well, so was intrigued to get his opinion on this. The doctor advised of a type of cisternogram that used radioactive dye and would be more efficient at picking up a leak. He advised he would write to my local neurologist to recommend they perform the scan back home.
The surgical repair
I finally went into hospital to have the pseudomeningocele and cavity at the back of my head repaired. My surgeon had shown me the implant at an outpatient appointment a week prior to the admission and explained he had sent it off to be sterilised after it had arrived from Germany. It was quite remarkable to know that it was custom made to fit the back of my head, and my surgeon was also very optimistic about the operation he was going to perform.
Shortly after I was admitted to the neurosurgery ward, I went in for surgery and my surgeon asked for my permission to take some photos of the procedure for a medical journal. I woke up a few hours after the operation and my surgeon said, “you will never have a problem with that pseudomeningocele again.” Whilst I was still in the hospital my surgeon carried out the scan recommended by the CSF leak expert in the Midlands, which thankfully showed there was no longer a leak of CSF at the back of my head. I found that I had relief almost immediately after I woke up following the operation. The only thing that was still prominent was the popping in my ears, which resolved when I was lying down.
One year onwards
My surgeon was so determined to resolve the issues and referred to one of his colleagues who suggested performing an Endoscopic Third Ventriculostomy (ETV), which is where a hole is made in the third ventricle of the brain so that CSF can drain. The ETV was carried out and my shunt was removed. This stabilised the pressure in my head and completely stopped the popping in my ears. I still suffer with the symptoms of the superficial siderosis but stopping the CSF leak has also stopped the bleed that caused the SS.
I have since had further ICP monitoring which has shown the pressure in my head is now normal, and a lumbar puncture has shown that there is now no blood in my CSF.
2025 Update - Which Came First? The Bleed or the Leak?


Life After Leak
Nearly nine years have passed since I had the diagnosis of infratentorial superficial siderosis (iSS) and things have somewhat settled in the sense that I no longer need anymore brain surgery. The CSF leak and bleed at the back of my head were both curbed when my neurosurgeon performed a cranioplasty, inserting a PEEK implant into the cavity and ‘obliterating’ the pseudomeningocele that was left following a brain tumour resection I had when I was 8 years old. Life now revolves around symptom management, which at times can be very difficult, but I feel it’s important to get the word out and emphasise how important it is to have a CSF leak repaired as soon as possible.
Symptom Management
Getting into a routine has been the key to managing iSS, but it all revolves around the symptoms and medication regime. I often find myself waking up at 5am just to regulate the symptoms such as the chronic constipation and fit my mediation in before having breakfast. Weekly neuro physiotherapy sessions are essential to maintain my mobility and battle the ataxia, dizziness and balance issues. Recently, after consulting Prof. Manjit Matharu I’ve found a way to control the chronic headaches by means of Botox injections, which I have every three months. The hearing loss and tinnitus can also be overwhelming, but having been completely deaf for 5 years, a cochlear implant has been lifechanging. It’s all become a way of life, and I’m still adapting and finding new ways to cope.
New Horizons
Thankfully, there are some positives, but again it’s a case of adapting to the new normal. In 2023 I took part in a ‘ParaTRYathlon’ for neurological patients at the neuro-physiotherapy centre I attend. It was during this event I found that I was able to cycle again, albeit on three wheels rather than two. It’s been a huge milestone for me and helped me to get out of the house, which was something I rarely did before. Pedal Power Cardiff is an all-inclusive cycling charity which models itself on cycling should be accessible for everyone and has not only helped me with my physical health, but my mental health too. I’ve met new people, I’m getting outside, and my confidence has grown so much.
Advocacy, Advocacy, Advocacy
Raising the profile of iSS is always on the agenda, and even when I was diagnosed in 2016 I did not for one minute believe it was a 1 in 3 million condition (which was the estimated prevalence at the time). A recent study of 10,305 images from the MRI brain biobank by a team at University College London Hospitals found 5 cases with features of iSS; and bearing in mind, there are probably others who have/had iSS that haven’t had a brain MRI. This suggests that the condition is less rare than once thought, with around a 1 in 2000 prevalence, bolstering the need for advocacy, awareness and research.
Raising the profile of infratentorial superficial siderosis is always on the agenda .... bolstering the need for advocacy, awareness and research.
